Quality Assurance and Performance Improvement
Category: Quality Assurance and Performance Improvement
ePoster Kiosk Presentation
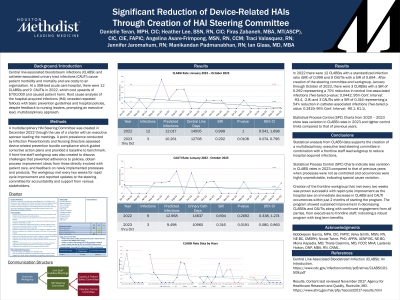
QAPI 154 - Significant Reduction of Device-related Hais Through Creation of HAI Steering Committee
Tuesday, June 4, 2024
12:46 PM - 1:15 PM CST
Location: Kiosk 3 - APIC Central, Hall 1
Has Audio

Danielle Teran, MPH, CIC
System Infection Preventionist
Houston Methodist
Presenter(s)
Disclosure(s):
Danielle Teran, MPH, CIC: No financial relationships to disclose
Background: Central line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTI) cause patient morbidity and mortality and are costly to an organization, averaging $13,000 to $48,000 per infection. At a 358-bed acute care hospital, there were 12 CLABSIs and 9 CAUTIs in 2022, which cost upwards of $700,000 and caused patient harm. Root cause analysis of the hospital-acquired infections (HAI) revealed repeated fallouts with basic prevention guidelines and hospital policies, despite feedback to nursing leaders, prompting an executive lead, multidisciplinary approach.
Methods: A charter was used to create a multidisciplinary HAI Steering Committee in December 2022 with an executive sponsor to lead the meetings. A point prevalence conducted by infection preventionists and nursing directors assessed device-related prevention bundle compliance which guided corrective action plans and provided a baseline to benchmark. A frontline staff workgroup was also created to discuss challenges that prevented adherence to policies, obtain process improvement ideas from those directly involved with patient care, and feedback on newly implemented processes and products. The workgroup met every two weeks for rapid cycle improvement and reported updates to the steering committee for accountability and support from various stakeholders.
Results: In 2022 there were 12 CLABSIs with a standardized infection ratio (SIR) of 0.999 and 9 CAUTIs with a SIR of 0.694 . After creation of the steering committee and workgroup, January through October of 2023, there were 3 CLABSIs with a SIR of 0.292 representing a 70% reduction in central line-associated infections (Two-tailed p-value: 0.0442; 95% Conf. Interval: -93.4, -2.8) and 3 CAUTIs with a SIR of 0.316 representing a 54% reduction in catheter-associated infections (Two-tailed p-value: 0.2419; 95% Conf. Interval: -90.1, 61.1).
Conclusions: Statistical analysis supports the creation of a multidisciplinary, executive lead steering committee in combination with a frontline staff lead subgroup to reduce hospital acquired infections.
Learning Objectives:
- Upon completion, participant will be able to list the building blocks on creating a multidisciplinary committee with robust executive involvement.
- Upon completion, participant will be able to describe the reasons a workgroup lead by frontline staff is essential in developing and implementing process improvement initiatives.
- Upon completion, participant will be able to conduct themselves as a liaison, bridging the gap between frontline staff challenges and executive patient safety goals.